TOPICS
For those new to this issue it’s best to know these terms before reading.
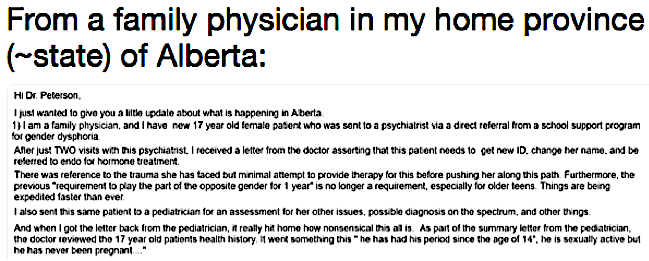
6) Lack of Gatekeeping: Minors Are Being Medically Transitioned without Meaningful Psychological Assessments
The shift in approach to youth presenting with gender distress is a result of the factors outlined below:
1) The result of the a study by Dutch researchers, de Vries et al. (2014) which seemed to illustrate that those with childhood-onset gender dysphoria who were well-screened prior to treatment seemed to improve with gender affirmation medical treatment.
2) The research from the Trans Youth Project that claim that their preliminary findings illustrate that social transition improves the mental health in trans identified youth.
3) The efforts by affirmation model activists who promote the positive findings of these studies, glossing over negative findings and the lack of long-term data.
4) The dissemination of a suicide narrative which lacks nuance, stating the increased risk of suicide in those who identify as transgender and that access to gender affirming care decreases this risk.
5) The promotion of glowing stories of trans children in the media and the lack of coverage of desisters, detransitioners or those who have been harmed by gender affirming care.
6) The promotion of positive attitudes towards medical transition in the media and negative attitudes about mental health screening, and proposing that any mental health comorbidities in the trans-identifying population is a result of “minority stress” due to being marginalized by society.
7) The lack of reporting of neurodevelopment conditions such as autism spectrum disorder or attention-deficit hyperactivity disorder, which cannot be attributed to “minority stress” associated with transgender identity.
As a result, many mental health and medical professionals are not doing any therapy or mental health screening in minors (cases verified in the United States, Canada and British private practices), including minors who have a sudden onset of gender dysphoria with no prior history. This is true whether or not this was the intention of all affirmation model advocates.
We acknowledge that access to treatment is a complicated issue and that there are reported harms from too much gatekeeping. Many trans people have reported excessive bureaucracy and wait times, and practices which they something they view as patronizing and a human rights violation. The most negative consequences of this can be seen in trans people who in desperation turn to unsafe methods of self-treatment.
An estimated 43.0% (95% confidence interval = 34.9, 51.5) of trans Ontarians were currently using hormones; of these, a quarter had ever obtained hormones from nonmedical sources (e.g., friend or relative, street or strangers, Internet pharmacy, herbals or supplements). Fourteen participants (6.4%; 95% confidence interval = 0.8, 9.0) reported currently taking nonprescribed hormones. Five indicated having performed or attempted surgical procedures on themselves (orchiectomy or mastectomy).
With the seriousness of some GD cases, and studies that indicate very low regret rates, it may be understandable why professionals want to allow easy transitions. It is important to keep in mind, however, that the clinicians from the GIDS in Britain point to the fact that these studies involved adults, often transitioned under a gatekeeping model, and that the demographics of those presenting with gender dysphoria has changed drastically. While those who accessed gender affirming treatments in the past were predominantly adult men, today, they are adolescent females and young children.
Long-term outcomes of GD management
In the UK, as yet there is little evidence of the longitudinal outcome from the GIDS. One published study showed that psychological support and puberty suppression were both associated with an improved global psychosocial functioning in adolescents with GD.22 One clear difficulty in tracking people is the frequent change in nominal and legal identity, including NHS number in those referred on to adult services and thus to date they have not been able to be followed up. The few longitudinal follow-up studies that have been published in the Netherlands have generally shown a high satisfaction outcome, particularly from those who have gone through surgical affirmation of their identified gender.23 24 These reported outcomes however are only from a highly selected group of fully dysphoric, well-adjusted individuals with few comorbidities and may not represent the full spectrum of gender diversity. Much further work needs to be done in this area.
Considering all of the current cohort of largely adolescent females with no prior history of gender dysphoria identifying as transgender, a more cautious model may be warranted. Unfortunately, even in Britain, where they have a protocol due to a public health system, as few as 4 sessions are required before gender affirming medical treatment is accessed.
The assessment period usually takes six months or more over a minimum of four to six sessions. At the end of the assessment, it may be possible to confirm or exclude a diagnosis of GD. Further treatment decisions are discussed with the family and agreed by the wider multidisciplinary team. One outcome may be to continue exploration of gender feelings and careful consideration of different developmental pathways and identity outcomes. A referral may also be made to the pediatric endocrinology team for consideration of puberty suspension with a gonadotropin-releasing hormone analogue (GnRHa) when the young person fulfils the minimum eligibility criteria, such as Tanner puberty stage 2.4 5 9 Once the pediatric team becomes involved, the child and family still continue regular sessions with their mental health clinician, and the two arms of the service work closely together. Following psychosocial assessment at the GIDS, on average 38%–40% of all clients attend the joint endocrine clinics, although this varies across the age range. Figure 2 highlights the age at which young people were referred to the GIDS, not the age at which they were referred to endocrinology (at a mean age of 14.4 years). The percentage referred at age 16 or 17 years is lower as many transition then to adult services to access physical treatment directly.
Similarly, a clinic in Australia (Australia Royal Children’s Hospital) requires only four sessions of mental health counselling before access to medical gender treatment is granted.
Following your initial assessment you will be offered four appointments with a child and adolescent clinical psychologist or psychiatrist and then a paediatrician both whom specialise in gender identity.
Affirmation model advocates have done a very good job of presenting the narrative that social transitions are an easy fix to mental health problems and that social transition has no real consequences. Further, these advocates posit that that trans identified children essentially have brains that match the opposite-sex brains. Thus, denying quick access to medical transition is unethical. As such, there have been many anecdotal reports of minors being immediately affirmed for medical transition, even if they had no childhood GD and have serious mental health issues. In Lisa Littman’s research, “Rapid Onset Gender Dysphoria” parents report the lack of assessment despite many youths having serious mental health issues prior to their trans identification, with therapist and doctors immediately affirming their child’s trans identification, including medically.
For parents who knew the content of their child’s evaluation, 71.6% reported that the clinician did not explore issues of mental health, previous trauma, or any alternative causes of gender dysphoria before proceeding and 70.0% report that the clinician did not request any medical records before proceeding. Despite all of the AYAs in this study sample having an atypical presentation of gender dysphoria (no gender dysphoria prior to puberty), 23.8% of the parents who knew the content of their child’s visit reported that the child was offered prescriptions for puberty blockers and/or cross-sex hormones at the first visit.
One participant described, “For the most part, I was extremely frustrated with providers NOT acknowledging the mental disorder, anxiety, depression, etc before recommending hormone replacement therapy.” And two participants described how the clinician treating their child’s gender dysphoria refused to speak with the patients’ primary care physicians. One participant said, “When we phoned the clinic, the doctor was hostile to us, told us to mind our own business. Our family doctor tried to reach our son’s new doctor, but the trans doctor refused to speak with her.” Another respondent shared “The pediatrician/‘gender specialist’ did not return calls or emails from the primary care physician who requested to talk with her about my son’s medical history before she saw and treated him…she disregarded all historical information provided by the family and primary care physician…did not verify any information provided by my…son at his first visit even after being provided with multiple other historical sources which differed significantly from his story.”
When asked about whether their child relayed their history completely and accurately to clinicians or whether they misrepresented or omitted parts of their history, of those who knew the content of their child’s visit, 84.2% of the parent respondents were reasonably sure or positive that their child had misrepresented or omitted parts of their history.
Littman summarizes several themes around behaviors of gender affirming therapists and doctors:
Theme: misrepresentation of information by the patient Several participants described how their child misrepresented their history to the clinician, thus, limiting the clinician’s ability to adequately explore mental health, trauma and alternative causes. One participant wrote, “At [the] first visit, [my] daughter's dialogue was well-rehearsed, fabricated stories about her life told to get [the] outcome she desired. She parroted people from the internet.” Another parent reported, “My son concealed the trauma and mental health issues that he and the family had experienced.” And a third parent said, “I overheard my son boasting on the phone to his older brother that ‘the doc swallowed everything I said hook, line and sinker. Easiest thing I ever did.’”
Theme: transition steps were pushed by the clinician. Some parents described clinicians who seemed to push the process of transition before the patient asked for it. One parent described that the doctor gave her daughter a prescription that she didn’t ask for, “The family doctor who gave her the Androgel Rx [prescription] did NOT ask her many questions (she was surprised by this), nor did he await her assessment by a licensed psychiatrist before giving her this Rx. Nor did she ask him for this Rx.” Another parent reported that she and her child were at the endocrinologist’s office only to ask questions, and described, “…[he] didn't listen to a word we were saying. He was too eager to get us set up with a ‘gender therapist’ to get the legal form he needed to start hormones, all while making sure we set up our next appointment within six months to start the hormones…”
Theme: parent views were discounted or ignored. Parents describe that the clinicians did not take their concerns seriously. One parent described, “I have to say I don't know, but it is hard to believe that they adequately examined the history of bullying and being ostracized for being different, and the autistic traits that would lend a person like my son to risk everything for identifying with a group. I know that in the few contacts I had with the providers, my concerns were discounted.” And another said, “All of our emails went unanswered and were ignored. We are left out of everything because of our constant questioning of this being right for our daughter [because of her] trauma and current depression, anxiety and self-esteem problems.”
Theme: parent had concerns about the clinicians’ competence, professionalism or experience. Parents expressed doubts about the clinicians regarding their experience, competence or professionalism. One parent said, “The clinic told me they explored these issues. I asked the risk manager at [redacted] if they'd considered a personality disorder. ‘Oh, no,’ she laughed. ‘That's only with the older patients, not the teenagers.’ I'm deeply suspicious of their competence.” Another parent described, “What does concern me is that the people she talked to seemed to have no sense of professional duties, but only a mission to promote a specific social ideology.”
Despite often immediate affirmation many of these youths, unlike those in the Dutch studies, did not improve,
The trajectories of the AYAs were not consistent with the narrative of discovering one’s authentic self and then thriving. Specifically, parents reported that, after “coming out,” their children exhibited a worsening of their mental well-being. Additionally, parents noted worsening of the parent-child relationship and observed that their children had narrowed their interests (Table 8). Although small numbers of AYAs had improvement in mental well-being (12.6%), parent-child relationship (7.4%), grades/academic performance (6.4%), and had broadened their interests and hobbies (5.1%); the most common outcomes were worsened mental well-being (47.2%); worsened parent child relationship (57.3%); unchanged or mixed grades/academic performance (59.1%); and a narrowed range of interests and hobbies (58.1%). One parent describing her child’s trajectory offered, “After announcing she was transgender, my daughter’s depression increased significantly. She became more withdrawn. She stopped participating in activities which she previously enjoyed, stopped participating in family activities, and significantly decreased her interaction with friends. Her symptoms became so severe that she was placed on medication by her physician.” Table 9 describes cumulative rates of mental illness and neurodevelopmental disability at the time of survey.
There was a subset of eight cases where parents described watching their child have declining mental well-being as they became gender dysphoric and transgender-identified and then had improving mental well-being as they dropped or backed away from a transgender-identification.
A post by The Gender Dysphoria Working Group (in a response to trans activist Julia Serano), point to other evidence corroborated Dr. Littman’s findings.
For example, Littman found that 62.5% of young people were diagnosed with one or more psychiatric disorder prior to announcing that they were trans. 48.4% had experienced stress or trauma. 45% were engaging in self-harm prior to coming out as trans and 58% had difficulties with emotion regulation. These proportions appear very high and suggest a troubled, clinical population. And concerningly, of those parents who were aware of the content of their child’s consultation with a mental health professional 71.6% reported that the clinician did not explore mental health issues, previous trauma or other potential causes for gender dysphoria. Littman reports: “The very high expectation that the majority of AYAs held that transition would solve their problems coupled with the sizable minority who became unwilling to work on their basic mental health issues before seeking treatment support the concept that the drive to transition might be used to avoid dealing with mental health issues and aversive emotions.”
Littman’s study corroborates what other clinicians around the world have been noting in recent years. For example, the Report of the American Psychiatric Association Task Force on Treatment of Gender Identity Disorder notes the following: “In the Toronto sample, there is significant psychopathology in the adolescent sample, particularly in the late-onset group. As indicated above, many of these adolescents also present with a shorter duration of cross-gender feelings and less clarity or consistency regarding the nature of their gender concerns as well as histories of trauma, psychosis, body dysmorphic disorder, and severe depression that seem related to their cross-gender feelings. Despite these observations, often these adolescents are very certain that SRS is the “only” solution to their dilemmas and because of this may become very pressuring of doctors in their quest for SRS. Access to internet sites that uncritically support their wishes appears to facilitate their intense desire for hormones and surgery”
Examples of cases of minors and young adults receiving immediate gender affirmation with zero or near zero mental health exploration.
Many people believe that minors in the United States (and elsewhere) are being put through an effective screening process and are not allowed to access hormones and surgeries until they are 16 (hormones) or 18 (surgery). They mistakenly think that psychologists are closely working with young people who have all known they were trans since childhood. This is often not the case. Further, surgeries are happening on minors as young as 13, even on youths presenting as trans only recently. Double mastectomy is legal in Oregon without parental consent. The cases presented demonstrate minors are being socially and medically transitioned with no psychological assessment . These cases are all verified to be real by us or by journalists writing news stories.
The below cases are particularly disturbing because therapists immediately affirmed trans identified minors (who often met persistent, insistent, and consistent criteria for over 6 months), often recommending medical treatments which have permanent effects.
In this case a trans enthusiastic school counsellor at a school went behind this desister mother’s back.
Carrie had a similar experience with her daughter, who had underlying learning difficulties. She told National Review, “In talking with my daughter, I discovered that she had brought the subject [transgenderism] up because of curiosity about other kids at school, and that her therapist had told her that curiosity means you are probably trans.”
“She had been told by the therapist not to tell me yet, because it takes parents a long time to ‘come around.’”
The therapist then denied this. But Carrie found messages on her daughter’s iPhone that confirmed the story. Her trust was shattered, and they took her daughter elsewhere.
“It’s been a year now since the revelation, and my daughter has completely moved on. But I’m terrified to think what fate might have befallen her. We would never in a million years have dreamt such things were going on inside that office while we waited outside.”
Another parent is Katherine. Her daughter first got the idea about transgenderism from a school presentation, at a small school where around 5 percent of the students believed themselves to be transgender. Katherine considered herself to be progressively minded and had chosen a school with such values in the hope that her child (who had some symptoms of autism) might feel included.
“Gender therapists told me not to question my daughter; that to do so was ‘insulting’ and that I must affirm her identity or she would be at high risk of suicide.”
Every therapist we spoke with – and we spoke with quite a few – told us that if a teen says they are trans, then they are, and the parents’ job is to affirm and help them transition. There was no therapist who would say to Abby, ‘This is not my experience of you.’ No therapist was interested in exploring the possibility that something other than being born into the wrong body could be operating here.
Like many who read this blog, I phoned gender therapists during the weeks after her announcement that she was trans. Without even meeting my child in the flesh, all four of these therapists talked to me like this trans thing was a done deal. I wrote about one of those conversations here. One very friendly therapist, who identifies as FtM and whose website stressed “his” commitment to “informed consent,” assured me that there was no need for my daughter to first experience a sexual or romantic relationship before deciding whether she was trans. “Most of the young people just skip that step now,” the therapist said...
This same therapist signed my kid up for a “trans teen” support group scheduled for the following week—again, without ever having met her. “There’s nothing you or I can do about your daughter being trans,” said another therapist… on the phone, without having met my kid. Yet another therapist refused to talk to me at all; insisting she’d have to have a private appointment with my kid first.
Here, a journalist reporting on gender dysphoria highlights cases of physicians putting minors on testosterone under apparently very unstable circumstances:
The first individual was very intelligent, but struggling socially, especially around girls. They were fixated on emphasising their femininity in selfies, leading the parents to suspect body dysmorphic disorder (a troubling belief that there is something wrong with one’s body). This individual’s boyfriend then came out as gay. Sometime following this, the client disclosed that they identified as a boy. This change in identity happened “overnight” with no developmental history of cross-gender identification.
The second client’s history is more convoluted: at around age 14-15 this individual had disclosed that they were transgender (now identifying as male), and had felt this way for a while. This individual also had a history of anxiety, social problems interacting with girls and extreme anxiety about sexuality. From the point of disclosing their gender dysphoria, they also reported that they were gay (oriented towards men), but had no interest in romantic/sexual relations.
In both these cases, after an initial assessment , the individual was given testosterone treatment by a physician against the wishes of the parents – in the first case, the physician actually refused to meet the parents, and in the second, the physician recorded that the issues raised by the parents regarding anxiety, sexual and social problems weren’t relevant for the course of action. Sadly, in the case of the second individual, a few months after the start of the hormone treatment, they made a suicide attempt that required hospitalization; the reasons for this were not reported.
Are the indicators of psychological vulnerability identified in these case histories the consequence, cause or simply coincident to gender identity disorder? If they are all solely a fall-out from the gender dysphoria, then the decisive approach of the physicians described above has a certain sense to it. But if some of the psychological complications pre-dated the gender dysphoria, or were separate from it, then at the very least this would suggest that the consulted physicians should have considered a broader treatment plan, and considered the psychological complications when judging their clients’ “readiness” to commence biomedical treatments
However, when a child with gender dysphoria is “insistent, persistent, and consistent” over an extended period, then (under the gender affirmative approach) this is typically treated as a good indicator that it is appropriate to begin facilitating the transition process. The trouble is, psychological vulnerabilities can also be persistent, and if a young person feels like they’ve found the solution, it’s understandable that they might not want to let go.
A parent in this news article corroborates an attitude of enthusiastic social and medical transition of minors without mental health screening, with some evidence some therapists are actually cheerleading medically transitioning minors, in this case one not asking for it. From the article, “The Sudden Surge of Transgender Teens.”
Another friend’s 14-year-old son began identifying as a trans girl last year but doesn’t present as female — doesn’t wear feminine clothes, have girl friends, or even shave, um, her mustache. So when multiple Los Angeles therapists urged them to start the kid on hormone replacement therapy, the parents resisted…“All of them are pushing our child down that road, and our child is not showing us that she wants to go down that road. It’s really dangerous,” says my friend — who is about as progressive as they come. “I mean, we don’t even let her eat chicken with hormones in it!
In this case Johanna Olson-Kennedy is not only not addressing mental health concerns in a youth, she is actively encouraging a tomboy female child, not expressing gender dysphoria, to consider the possibility she is trans since she likes short haircuts and boy’s clothes. By the end of the visit a child who was not identifying as transgender now believes she is a boy. Olson proclaims “I just gave him the language.”
A story from a parent sent to Thehomoarchy.com blog about the rush to transition minors and view parents with hostility.
After I posted this some parents contacted me who have a daughter who had no history of childhood dysphoria. She had been hospitalized for being suicidal twice as a tween but not because of dysphoria. She suddenly came out as trans a couple of years later, lied to the gender therapist about key issues and is starting testosterone as a minor. The parents were told to put them on testosterone at the first appointment. The gender therapist never asked the parents about depression or anxiety possibly contributing to this. The GT interviewed the parents to deem them “oppressor” or “non-oppressor” in their words. This was during only one meeting where they never asked the parents for any input about the child’s history. The youth said they were confused before they went into therapy and within a very short time was starting testosterone. These parents were shocked at the speed of which their minor was affirmed as needing drastic medical intervention with permanent effects.
Another mother from London said an NHS mental health expert refused to listen to her protests that her 13-year-old daughter’s issues were not really about her gender.
The teenager told her parents in July 2016 that she wanted to be a boy and was referred by her GP to CAMHS, attending her first appointment in January this year.
Her mother told the psychologist she believed her daughter was suffering from anxiety. The 47-year-old said she also thought her daughter had been heavily influenced by messages sent to her by other adolescents on social media. She said: ‘One said she should tell me she will drink bleach if we don’t let her become a boy.’
But the psychotherapist still continued to push the parents to refer to their child as ‘he’ and even allow the teen to bind her chest. The mother added: ‘They just weren’t listening to the one person who knows their child best. I was saying, “I know her – you don’t.”’ A month ago the mother took her daughter to a private mental health service where the psychologist shared her scepticism about the girl wanting to change sex.
The youngster now rarely mentions wanting to be a boy.
We include some examples of young adults. While we fully acknowledge adult’s rights to transition, we believe that the rising numbers of young adult females might call for greater caution as this group may be at more at risk for later regret. We hope the trans community will promote good mental health support for all young adults given they don’t reach full maturation as evidence by brain studies indicate, until late into the 20’s. This is all for the sake of the health of the community given mental illness and suicide ideation remain high post medical transition.
After a 30-minute consultation with a physician’s assistant, Molly was given an appointment for the following week to begin testosterone injections. There was no exploration of her other physical and mental health issues, and whether these may have influenced her belief that she was trans. There was also no caution expressed about how hormone treatment might affect Crohn’s disease. Molly simply had to sign a consent form stating that she identified as male and understood the risks associated with testosterone.
The PA (physician assistant) also suggested that Molly schedule top surgery – a double mastectomy – within a few months. When Claire stated that she and Jeff wanted time to do research and consider alternatives before allowing Molly to begin taking testosterone or have surgery, the PA told her that their job as parents now was to support and affirm their ‘son.’ In front of Molly, he told Claire she ought to get her own therapist to deal with her issues so that she could be a better support person to ‘Max.’ When Claire and Jeff expressed concerns about Molly’s anxiety and isolation, the PA stated that these were likely a result of Molly being transgender, and would resolve once she began to transition.
The rest of Molly’s story is not a happy one. At the end of her freshman year, she had top surgery, paid for by student health insurance. She moved back home over the summer so that her parents could help during her recovery. By this time, Molly’s voice had deepened, facial hair had grown in, and she passed as male full-time. Molly had become Max.
This case involves an adult on the autism spectrum with a maturity level of a nine-year-old. This person was immediately affirmed and medically transitioned. The young, developmentally disabled female had serious health consequences.
Shortly afterwards, at a meeting of the group called PFLAG (Parents and Friends of Lesbians and Gays), she met other transgender teens, along with a “gender therapist.”
The “gender therapist” gave the go-ahead for her daughter’s “transition” after only two meetings, the mothersaid…
Levinstein’s daughter’s double mastectomy took place a year ago and she is now on an aggressive regimen of additional testosterone. When the endocrinologist gave her daughter the first batch of testosterone, it came with 30 pages of warnings and said that the medical profession does not know of the long-term health risks associated with such a regimen. Her daughter also has Crohn’s disease and has been hospitalized several times for what she describes as “absorption issues” related to the testosterone…
This case involves another young adult (18) but the lack of mental health exploration has created a cautionary tale:
In spite of having transitioned, Max did not blossom into his “authentic self.” In fact, his mental health worsened. He was more anxious and isolated than ever and rarely left the house, spending most of his time online. He told his mother that he feared people would know he was trans and try to harm him were he to go out in public. When Claire tried to reassure him by offering to accompany him, Max often refused, expressing a lack of trust for Claire and her motives because, in Max’s words, Claire was a “transphobe.” “I feel as though my child has been taught to be paranoid about me,” Claire told me.
By the end of that summer, Max had yet another diagnosis to contend with. He began experiencing symptoms of interstitial cystitis (IC), a painful and often debilitating condition that affects the bladder. Claire was not able to find any discussion in the medical literature about testosterone use and interstitial cystitis, but she did find online accounts of trans men suffering from worsening IC symptoms after going on testosterone. Claire pointed out that we just don’t know enough about how these medications affect people long-term. “I would say these gender doctors are experimenting on people,” Claire told me, “but when you experiment, you keep data and track outcomes.
The below cases are anecdotal and cannot be verified as many people discussing this on social media must remain anonymous to protect themselves, their livelihoods, and their children from a very angry identity politics environment.
This parent shares her experience in which all of the professionals around her daughter immediately affirm her as trans. No professionals suggested the youth avoid drastic medical intervention and explore being comfortable as a lesbian. The story is consistent with the many others already presented. This is a case in which the young person outgrew their GD, becoming comfortable in her own body. It is one of many examples as to why the youth gender medical reassignment movement is a danger to lesbian (and gay) teenagers.
Below are more screen captures of social media posts of the lack of appropriate assessment or exploration of the gender distress.
While some clinicians offer only an affirmation approach, others hold space for their patients to grow and come to a broader understanding of their gender distress. There are cases of desistance where the therapist helped by not enthusiastically affirming.
Even though the affirmation model/ informed consent model in regards to minors is sweeping the mental health and medical community, and anti-conversion therapy laws are being written to prevent working through alternative coping methods before medical transition, there are cases where therapy does, in fact, resolve the youths gender confusion and angst, even when the gender dysphoria is severe helping the youth to realign with their biological sex. Some therapists are alarmed by the passage of anti-conversion therapy laws because they feel it limits they ways they can explore the youth’s identity.
Abigail’s story involving parents who did not immediately medically transition their child despite professional advice. Every single therapist affirmed this child as transgender.
Instead, Marci and James started talking more to Abigail about all the anxiety she was experiencing in her life. It soon became clear to all three that she was using a trans identity as a way of coping with the anxiety. Talking through it, over time, Abigail became calmer and more relaxed.
With her parents’ love and support, Abigail has backed away from identifying as trans. Marci and James report that she seems happier and less anxious. They feel relieved that Abigail appears to have avoided a course of action that would have led to medical intervention. But they are cautious.
“For now, she is happier in her own skin,” Marci said. “But in this culture today, it’s very hard to be a girl.”
Other stories, such as the one reported here describes youth who desisted after receiving proper mental health counseling. This youth met diagnostic criteria for medical transition in many places in the United States, demonstrating the risks of the affirmation model, calling into question whether the DSM criteria is sufficient to use in determining whether one is a good candidate for medical affirmation.
“Other stuff” mostly meant her problems with anxiety and depression. Edwards-Leeper told Jenny and Delta that while Delta met the clinical threshold for gender dysphoria, a deliberate approach made the most sense in light of her mental-health issues.
“At the time I was not happy that she told me that I should go and deal with mental stuff first,” Delta said, “but I’m glad that she said that, because too many people are so gung ho and just like, ‘You’re trans, just go ahead,’ even if they aren’t—and then they end up making mistakes that they can’t redo.” Delta’s gender dysphoria subsequently dissipated, though it’s unclear why. She started taking antidepressants in December, which seem to be working. I asked Delta whether she thought her mental-health problems and identity questioning were linked. “They definitely were,” she said. “Because once I actually started working on things, I got better and I didn’t want anything to do with gender labels—I was fine with just being me and not being a specific thing.”
In this article a therapist who promotes a mental health exploration indicating that she has had young people resolve their gender issues through exploration. While some may argue this is inappropriate, the option of exploration vs life long hormonal treatment and possible surgery should be a choice available to patients. The consideration of the potential side effects, health risks, financial/social/emotional costs, and life-long consequences should not be overlooked, and it is not in the best interest of the young person dismiss this perspective without due consideration.
© Gender Health Query, 6/1/2019
REFERENCES FOR TOPIC 6
Updates Topic 6
CONTINUE TO TOPIC 7:
Conversion therapy laws: impacts for trans youth vs gay youth who don't need medical treatment
Conversion therapy laws are being used to ensure that mental health professionals validate the trans identity of the growing numbers of trans-identified minors.
Contents
6) Examples of minors being medically transitioned without any meaningful psychological assessments
-2 Cases of desistance where the therapist helped by not enthusiastically affirming
BACK TO OUTLINE
More
1. Do Children Outgrow Gender Dysphoria?
3. Are children & teens old enough to give consent?
4. Comments safety / desistance unknown
5. Gender dysphoria affirmative model
6. Minors transitioned without any psychological assessments
8. Regret rates & long term mental health
11. Why are so many females coming out as trans / nonbinary?
13. Why is gender ideology being prioritized in educational settings?
14. Problems with a politicized climate (censorship, etc)