Sensitive Topics: Suicide Risk Information Updates
NEWS COMMENTARY
We are updating GHQ with some more studies on the important topic of suicide risk in gender dysphoric minors and adults.
Studies on Trans Mental Health and Suicide Risk
We are adding information about an older study (Kuiper 1988) (no online link available).
141 Dutch TS: 36FtM, 105MtF.
Recruitment through letters and ads.
Followed up: 11 FtM, 50 MtF.
42 lost to follow up.
No control group.
Findings: Suicide attempt before treatment FtM 19%, MtF 23.6%. 3 MtF completed suicide since surgery.
Unemployment: 36% FtM, 60% MtF.
No association between well-being and phase of treatment .
11% were unhappy with treatment.
“SRS is no panacea” study authors claim.
We are adding some comments about another older study (Lauder 1998) (no online link available):
They compared MtF (134) vs FtM (99) 1972-1992.
MtF were older, had a history of marriage, more likely heterosexual.
FtM had increased cross gender behavior in childhood.
Mean age of request of surgery=31.
MtF had increased fetishism.
Suicide attempt MtF 14.1%, FtM 23.1%
Mood disorder MtF 7.1%, FtM 12.7%
Personality Disorder MtF 7.1%, FtM 14.9%
This study indicates that despite medical transition, the females retain higher levels of suicide attempts and personality disorders, consistent with their biological sex, not gender identity, versus males.
Murad et al., 2010 is an older review study. They describe their study as a review of “low quality” evidence due to study designs. What is relevant to our site here is that yes, medical transition shows improvement for a majority of adult transitions. But there is still a significant minority (see QOL data) who may not be helped. This is relevant in regards to minors transitioning medically.
Some findings:
Resolution of gender dysphoria
Pooling across studies shows that after sex reassignment, 80% ofindividuals with GID reported significant improvement in genderdysphoria (95% CI = 68–89%; 8 studies;I2= 82%). Proportion inMF subgroup is 71% (41–93%) and in FM subgroup is 86% (65–98%).
function (95% CI = 60–81%; 15 studies;I2= 78%). This propor-tion in MF subgroup is 63% (45–79%) and in FM subgroup is 80%(68–89%)…
Psychiatric comorbidities
Pooling across studies shows that after sex reassignment, 78%of individuals with GID reported significant improvement in psychiatric symptoms (95% CI = 56–94%; 7 studies;I2= 86%).This proportion in the MF subgroup is 70% (33–96%) and inthe FM subgroup is 84% (73–92%).
Psychiatric comorbidities were fairly prevalent in individuals with GID…
Suicide attempt rates decreased after sex reassignment butstayed higher than the normal population rate…
Quality of life
Pooling across studies shows that after sex reassignment, 80% ofindividuals with GID reported significant improvement in qualityof life (95% CI = 0Æ72–0Æ88; 16 studies;I2= 78%). This proportionin the MF subgroup is 84% (68–95%) and in the FM subgroup is78% (67–87%)…
Satisfaction with sexual function
Pooling across studies shows that after sex reassignment, 72% ofindividuals with GID reported significant improvement in sexual function (95% CI = 60–81%; 15 studies;I2= 78%). This propor-tion in MF subgroup is 63% (45–79%) and in FM subgroup is 80%(68–89%).
A survey (Clark 2014) from New Zealand indicates social contagion in trans identity (1.2% of the respondents are categorized as trans and 2.5% “are not sure”). The study found being a trans-idenitified youth was associated with: a parent not caring, depression, and suicide attempts. 40% had engaged in self injury and 20% made a suicide attempt in the last 12 months. 20% said they were bullied.
(Reisner 2015) is another study on trans youth showing higher rates of mental health problems and suicide risk. Unlike some other studies they didn’t find significant differences based on sex:
Results
The sample (N = 360) had a mean age of 19.6 years (standard deviation, 3.0); 43% white, 33% racial/ethnic minority, and 24% race/ethnicity unknown. Compared with cisgender matched controls, transgender youth had a twofold to threefold increased risk of depression, anxiety disorder, suicidal ideation, suicide attempt, self-harm without lethal intent, and both inpatient and outpatient mental health treatment (all p < .05). No statistically significant differences in mental health outcomes were observed comparing FTM and MTF patients, adjusting for age, race/ethnicity, and hormone use.
Conclusions
Transgender youth were found to have a disparity in negative mental health outcomes compared with cisgender youth, with equally high burden in FTM and MTF patients. Identifying gender identity differences in clinical settings and providing appropriate services and supports are important steps in addressing this disparity.
Tucker et al., 2018 is an odd study that shows a lowering of suicide risk with full surgery and hormone transition but not each one alone where the outcomes may be worse:
This study doesn’t reference suicide specifically but shows a much higher percentage of comorbid mental health conditions in trans people. This study is useful because so many studies on the trans population are survey volunteer studies or have huge lost to follow-ups. This study comes from an electronic health record study.
A new study on suicide risk has come out of the Netherlands noting, like others, trans people have an elevated risk of suicide. The study has a 36% lost to follow-up rate, a major issue with many studies on transgender people. Four of the suicides were people who presented to the healthcare system first as children. Females who transition have a 5x risk of suicide compared to other females; men who transition have a 3x risk of suicide compared to other males. The authors focus on absolute risk of suicide and promote a theory that because FtMs have a higher social status than MtFs they have lower rates of suicide. In reality, MtFs are male, and this pattern is actually reflecting biological sex, not gender identity.
Results: Out of 5107 trans women (median age at first visit 28 years, median follow-up time 10 years) and 3156 trans men (median age at first visit 20 years, median follow-up time 5 years), 41 trans women and 8 trans men died by suicide. In trans women, suicide deaths decreased over time, while it did not change in trans men. Of all suicide deaths, 14 people were no longer in treatment, 35 were in treatment in the previous two years. The mean number of suicides in the years 2013-2017 was higher in the trans population compared with the Dutch population.
Conclusions: We observed no increase in suicide death risk over time and even a decrease in suicide death risk in trans women. However, the suicide risk in transgender people is higher than in the general population and seems to occur during every stage of transitioning. It is important to have specific attention for suicide risk in the counseling of this population and in providing suicide prevention programs.
Dr. Progovac reviewed Medicaid data to compare trans populations to people who are not trans.
“Disparities in Suicidality by Gender Identity Among Medicare Beneficiaries:”
Results: Gender minority beneficiaries had higher unadjusted suicidality than non−gender minor- ity beneficiaries in the disabled cohort (18.5% vs 7.1%, p<0.001). Significant suicidality predictors in all 4 groups included the following: age (except in older adult gender minorities), Medicaid eligible- ity, depression or behavioral health conditions, avoidable hospitalizations, and violence victimiza- tion. In age- and mental health−adjusted logistic regression models, gender minorities had higher odds of suicidality than non−gender minority beneficiaries (disabled, OR=1.95, p<0.0001; older adult, OR=2.10, p<0.0001). Disparities were not attenuated after adjusting for Medicaid eligibility, race/ethnicity, or region.
The Royal Children’s Hospital of Melbourne standards of care document claims high rates of mental health problems and suicide risk in the trans population:
A study of the mental health of trans young people living in Australia found very high rates of ever being diagnosed with depression (74.6%), anxiety (72.2%), post-traumatic stress disorder (25.1%),
a personality disorder (20.1%), psychosis (16.2%) or an eating disorder (22.7%). Furthermore 79.7% reported ever self-harming and 48.1% ever attempting suicide.7
“Deficiencies in Scientific Evidence for Medical Management of Gender Dysphoria” is a paper from a Catholic Medical Association and questions the efficacy of medical transition to reduce suicide risk in the long run:
Limitations of the existing transgender literature include general lack of randomized prospective trial design, small sample size, recruitment bias, short study duration, high subject dropout rates, and reliance on “expert” opinion. Existing data reveal significant intervention-associated morbidity and raise serious concern that the primary goal of suicide prevention is not achieved. In addition to substantial moral questions, adherence to established principles of evidence-based medicine necessitates a high degree of caution in accepting gender-affirming medical interventions as a preferred treatment approach. Continued consideration and rigorous investiga- tion of alternate approaches to alleviating suffering in people with gender dysphoria are warranted.
This review study (Surace 2019) of suicide risk in trans-identified youth endorses the affirmative model:
A random-effects meta-analysis was computed for the following outcomes: non-suicidal self-injury (NSSI), suicidal ideation and suicide attempts. Overall, we found a mean prevalence of NSSI of 28.2% (9 studies, 3057 participants, 95% CI 14.8–47.1). A similar prevalence (28%) was found for suicidal ideation (6 studies, 2249 participants, 95% CI 15–46.3), while the prevalence of suicide attempts was 14.8% (5 studies, 1039 participants, 95% CI 7.8–26.3). Subgroup analyses revealed no significant differences according to biological sex. Given the prevalence of suicidal behaviors in gender non-conforming youths, it appears desirable to implement therapeutic and support strategies for this population. Moreover, educational interventions directed to parents, teachers, mental health professionals and general community should be promoted to struggle against stigma and social isolation, factors that may contribute to increasing the risk of suicidal behaviors.
“Understanding the mental health of transgender and nonbinary youth” is a convenience sample and thus not the highest quality study:
Researchers examined responses from a national quantitative cross-sectional survey of more than 25,000 lesbian, gay, bisexual, transgender, queer, and questioning youth, aged between 13 and 24 years, in the US to better understand the mental health of transgender and nonbinary youth. Compared with cisgender lesbian, gay, bisexual, queer, and questioning youth, transgender and nonbinary youth were at increased risk of experiencing depressed mood, seriously considering suicide, and attempting suicide. Within-group analyses highlighted especially heightened risk for negative mental health outcomes among transgender males and nonbinary youth assigned male at birth. Findings point to the need to tackle transgender and nonbinary youth's needs specifically in prevention and intervention programs, and to promote policies that eliminate discrimination and victimization based on sexual orientation or gender identity.
29.7 % of trans and non-binary youth said they had been physically threatened. 82.8” per cent reported a depressive mood, 54.2 per cent had seriously considered suicide, and 28.6 per cent had attempted suicide.
Hughto et al., 2020 shows post medical transition suicide risk is lower than pre transition:
Nearly all participants (98.6%) reported disclosing their gender identity to family or a coworker; 67.4% endorsed recently using hormones, and 31.3% endorsed a gender-affirming medical procedure. In multivariable models, participants were at greater odds of NSSI, contemplating suicide, and attempting suicide before initiating the gender affirmation process compared to after.
A Swedish paper, “ The Evolution of the Diagnosis of Gender Dysphoria” (off line) reviewed data of the trans population in Sweden:
Suicide Mortality
Since 1998, a total of 6,334 persons have been diagnosed with gender dysphoria in Sweden. Of these, a total of 21 men and 18 women (registered sex at birth) have died from suicide. This represents 0.6 percent mortality by suicide among persons with a gender dysphoria diagnosis since 1998.
Studies and Discourse that May be Flawed.
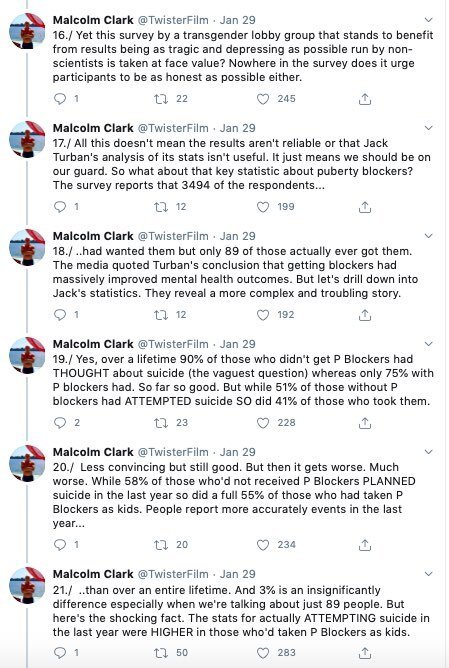
Jack Turban is a pro pediatric transition psychiatry student from Harvard. His studies have received a lot of criticism for confirmation bias. He has produced a new study, “Pubertal Suppression for Transgender Youth and Risk of Suicidal Ideation” that also seems to have problems with confirmation bias. Here are the claimed results about puberty blockers decreasing suicide risk:
RESULTS: Of the sample, 16.9% reported that they ever wanted pubertal suppression as part of their gender-related care. Their mean age was 23.4 years, and 45.2% were assigned male sex at birth. Of them, 2.5% received pubertal suppression. After adjustment for demographic variables and level of family support for gender identity, those who received treatment with pubertal suppression, when compared with those who wanted pubertal suppression but did not receive it, had lower odds of lifetime suicidal ideation (adjusted odds ratio = 0.3; 95% confidence interval = 0.2–0.6).
CONCLUSIONS: This is the first study in which associations between access to pubertal suppression and suicidality are examined. There is a significant inverse association between treatment with pubertal suppression during adolescence and lifetime suicidal ideation among transgender adults who ever wanted this treatment. These results align with past literature, suggesting that pubertal suppression for transgender adolescents who want this treatment is associated with favorable mental health outcomes.
Oxford sociology professor Micheal Biggs published a paper listing a myriad of problems with the study
If one looks more closely at the data, one finds that some of the categories are lower (such as ideation), but the total actual attempts and attempts resulting in need for inpatient care were higher with the group given puberty blockers which calls into question the claim in the conclusion. A suicide attempt requiring hospitalization could be considered more highly motivated:
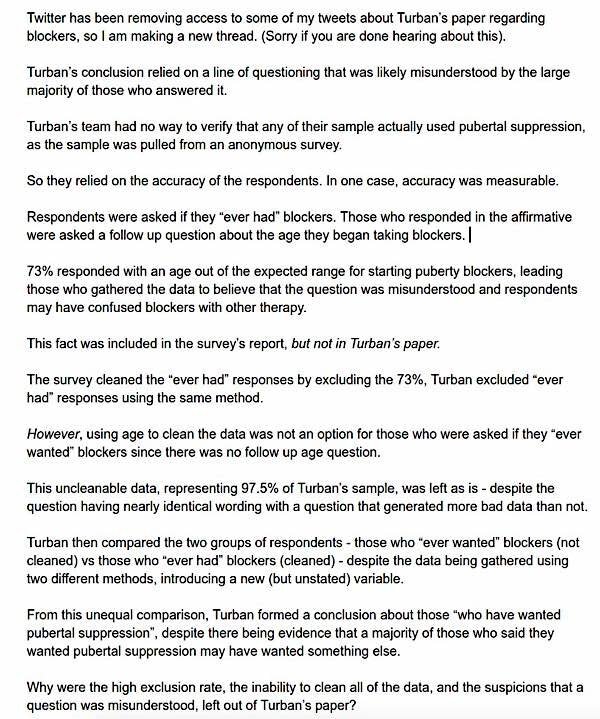
It also appears the sample of those who reported being given puberty blockers isn’t even reliable. Another commentator pointed out several other issues with the study. This commentator has been analyzing the research regarding the athletic superiority of MtFs, who are being put on girl’s and women’s sports teams, over females:
There is also no evidence it was the puberty blockers that affected different measurements on these questions. Younger people would have been more likely to have the option for puberty blockers, and trans acceptance has improved in the the last decade. Better measurements could be due to increasing acceptance. Not the puberty blockers. It is also a survey study and not likely to record the mental health outcomes of transition regretters, which may be a small number but would affect the mental health outcome data.
Malcom Clark is a science journalist and filmmaker. He is critical of this study. He commented in a long Twitter thread about flaws in how studies are presented. The whole thread can be found here, and it is worth reading:
Pediatrician Julia Mason, a Gender Health Query advisory board member, wrote a response regarding health professionals who believe they are saving lives (see article in Medscape) by advocating the gender affirmative model for minors:
What has really struck me in conversations with and observations of doctors providing puberty blockers and cross-gender hormones to gender dysphoric youth is their utter conviction that they are saving lives.
"Would you rather have a dead daughter, or a live son?"Kevin Wang MD says suicide attempts are 9 to 10x higher.
But when you look at the data, the rates of suicide and self harm are "more similar than different" to the rates of youth referred for other mental health concerns. I'm quoting from @ZUCKERKJ's excellent article from earlier this year.
Study on LGB Youth who are also at risk.
Recently a study was done on suicide risk and LGB youth taken from data from The Trevor project (and LGBT youth organization) and CDC.
“Suicidality Disparities by Sexual Identity Persist from Adolescence into Young Adulthood” shows that bisexuals at higher risk than gay and lesbian youth. This is similar to findings in other studies on bisexuals.
LGBT media sites like to make statements blaming all mental health problems on bigotry. From Out Magazine:
But, according to experts, these statistics come as a result of a worsening culture of anti-LGBTQ+ legislation and sentiment from political and religious leaders.
The Trevor Project researcher also blames all mental health problems on stigma:
“Here’s what we know: young LGBTQ people are not prone to suicide because of their sexual orientation or gender identity,” Dr. Amy Green, The Trevor Project’s director of research, tells Out. “They are at a higher risk of suicidality because of increased experiences of internalized stigma, discrimination, and rejection from others. No one factor causes an individual to attempt suicide, but the cumulative effect of these stressors can be detrimental to one’s mental wellness and increase the risk for suicidal ideation. According to The Trevor Project's 2019 National Survey on LGBTQ Youth Mental Health, 76 percent of LGBTQ youth felt that the recent political climate impacted their mental health or sense of self.”
While there is little debate bigotry, stigma, and family rejection harm mental health, it would be useful for these researchers to expand their understanding of what is going on rather than narrowly focus on points that validate an LGBT activist narrative. For example, there may be other personality traits involving bisexuals that cause more mental health problems rather than just stigma, as LG youth also deal with stigma bet have better overall mental health. Social media likely has an effect of worsening mental health for LGBT youth as these online spaces fuel paranoia and victim complexes, which may be socially reinforcing and contagious. Mental health is worsening even for female heterosexual teens.
REFERENCES
Biggs, M. (2020). Puberty Blockers and Suicidality in Adolescents Suffering from Gender Dysphoria. Archives of Sexual Behavior. doi:10.1007/s10508-020-01743-6
Clark, T.C., Lucassen, M.F.G., Bullen, P., Denny, S.J., Fleming, T.M., Robinson, E.M., Rossen, F.V. (2014). The Health and Well-Being of Transgender High School Students: Results From the New Zealand Adolescent Health Survey (Youth'12). Journal of Adolescent Health 55(1), 93-99. doi: 10.1016/j.jadohealth.2013.11.008.
Firth, S. (2019, September 24). AAFP Debates Care for Transgender Youth. Medscape. Retrieved from https://www.medpagetoday.com/meetingcoverage/aafp/82347
Guerrero, D. (2020, February 11). Study: LGBTQ+ Youth are Four Times More Likely to Attempt Suicide. Out. Retrieved from https://www.out.com/health/2020/2/11/study-lgbtq-youth-are-four-times-more-likely-attempt-suicide
Hughto, J.M.W., Gunn, H.A., Rood, B.A., Pantalone, DW. (2020). Social and Medical Gender Affirmation Experiences Are Inversely Associated With Mental Health Problems in a U.S. Non-Probability Sample of Transgender Adults. Archives of Sexual Behavior. doi: 10.1007/s10508-020-01655-5
Hruz, P.W. (2019). Deficiencies in Scientific Evidence for Medical Management of Gender Dysphoria. The Linacre Quarterly. doi.org/10.1177/0024363919873762
Kim, B. (2020, January 28). Jonathan Haidt on Social Media-Driven Anxiety Among Kids. Retrieved from https://drbenkim.com/social-media-anxiety-kids-jonathan-haidt.htm
Murad, M.H., Elamin, M.B., Zumaeta, M.G., Mullan, R.J., Murad, A., Erwin, P.J., Montori, V.M. (2010). Hormonal therapy and sex reassignment: a systematic review and meta-analysis of quality of life and psychosocial outcomes. Clinical Endocrinology 72(2), 214-231. doi.org/10.1111/j.1365-2265.2009.03625.x
Price-Feeney, M., Green, A., Dorison, S. (2020). Understanding the Mental Health of Transgender and Nonbinary Youth. Journal of Adolescent Health 66(6), 684-690. doi.org/10.1016/j.jadohealth.2019.11.314
Progovac et al. (2020). Disparities in Suicidality by Gender Identity Among Medicare Beneficiaries. American Journal of Preventive Medicine 58(6), 789-798. doi.org/10.1016/j.amepre.2020.01.004
Reisner, S.L, et al. (2015). Mental Health of Transgender Youth in Care at an Adolescent Urban Community Health Center: A Matched Retrospective Cohort Study. Journal of Adolescent Health 56(3), 274-279. dio:https://doi.org/10.1016/j.jadohealth.2014.10.264
Ross, D. (2020, January 9). Teenager took his own life at hotel while awaiting autism diagnosis. Teeside Live. Retrieved from https://www.gazettelive.co.uk/news/teesside-news/marton-teenager-took-life-hotel-17532276
Surface, T., Fusar-Poli, L., Vozza, L. Lifetime prevalence of suicidal ideation and suicidal behaviors in gender non-conforming youths: a meta-analysis. European Child & Adolescent Psychiatry. doi.org/10.1007/s00787-020-01508-5
The Trevor Project. (2020, February 6). Suicidality Disparities by Sexual Idenity Persist from Adolescence into Young Adulthood. Retrieved from https://www.thetrevorproject.org/2020/02/06/suicidality-disparities-by-sexual-identity-persist-from-adolescence-into-young-adulthood/
The Royal Children’s Hospital of Melbourne Standards of Care. Retrieved from https://www.rch.org.au/uploadedFiles/Main/Content/adolescent-medicine/australian-standards-of-care-and-treatment-guidelines-for-trans-and-gender-diverse-children-and-adolescents.pdf
Tucker, R.P., Testa, R.J., Simpson, T.L., Shipherd, J.C. Hormone therapy, gender affirmation surgery, and their association with recent suicidal ideation and depression symptoms in transgender veterans. Psychology Medicine 48(14), 2329-2336. doi.org/10.1017/S0033291717003853Pub
Turban, J. L., King, D., Carswell, J. M., & Keuroghlian, A. S. (2020). Pubertal Suppression for Transgender Youth and Risk of Suicidal Ideation. Pediatrics, Feb;145(2):e20191725. doi:10.1542/peds.2019-1725
Wanta, J.W., Niforatos, J.D., Durbak, E., Viguera, A., Altinay, M. (2019). Mental Health Diagnoses Among Transgender Patients in the Clinical Setting: An All-Payer Electronic Health Record Study. Transgender Health. 4(1). doi.org/10.1089/trgh.2019.0029
Wiepjes, C. M., Heijer, M. den, Bremmer M.A., Nota N. M., Blok C. J. M. de, Coumou, B. J. G., Steensma, T.D. (2020). Trends in Suicide Death Risk in Transgender People: Results From the Amsterdam Cohort of Gender Dysphoria Study (1972-2017). Acta Psychiatry Scandinavia Feb 18 (ahead of print). doi: 10.1111/acps.13164
Wigzell, O. (2020, February). The Evolution of the Diagnosis of Gender Dysphoria. Socialstyrelsen.